Advisory Board Company includes Carevive in a report detailing four tactics to improve quality and patient experience while reducing costs
As published in The Advisory Board Company website.
Improving care at the end-of-ife is a prime opportunity for cancer programs to drive quality, decrease costs, and enhance the patient and family experience.
Aggressive end-of-life care that provides no clinical benefit, including chemotherapy and hospitalizations in the last two weeks of life, contributes significantly to overall costs of care. In addition, it often negatively impacts patients’ and their families’ quality of life and care experience.
While improving end-of-life care has been a longstanding priority in the oncology community, it remains challenging due to cultural and clinical barriers. To help cancer program leaders overcome these challenges, this report outlines four tactics:
- Empower patients to start the conversation
- Give the care team the right tools
- Integrate palliative care early
- Build better hospice relationships
Carevive is featured in the Tactic #2 Section: Give the care team the right tools.
The profile on Carevive features a case study of University of Alabama Medicine (UAB), an NCI-designated Comprehensive Cancer Center based in Birmingham, Alabama. UAB partnered with USA Mitchell Cancer Institute (Mobile, Alabama) and AtlantiCare Cancer Institute (Egg Harbor Township, New Jersey) to conduct a study with Carevive. They used Carevive’s patient care planning platform to provide physicians with a tool that auto-generates a patient care plan and triggers appropriate referrals across the cancer continuum based on clinical data, patient-reported outcomes, and evidence-based guidelines.
To standardize advance care planning for all patients, UAB Medicine, AtlantiCare Hospital, and the USA Mitchell Cancer Center are using Carevive, a treatment planning platform. These organizations are also participating in the Oncology Care Model (OCM), which requires comprehensive treatment plans, which include advance care plans, for all patients.
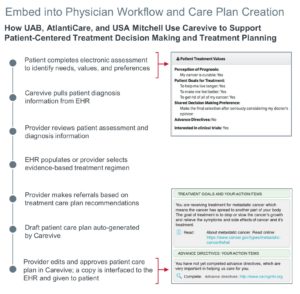
How UAB, AtlantiCare, and USA Mitchell Use Carevive to Support Patient-Centered Treatment Decision Making and Treatment Planning
Using patient-reported and clinical data, the tool guides providers to select an evidence-based treatment regimen. It also prompts physicians to ask patients about their treatment goals and alerts physicians when patients do not have an advance care plan documented.
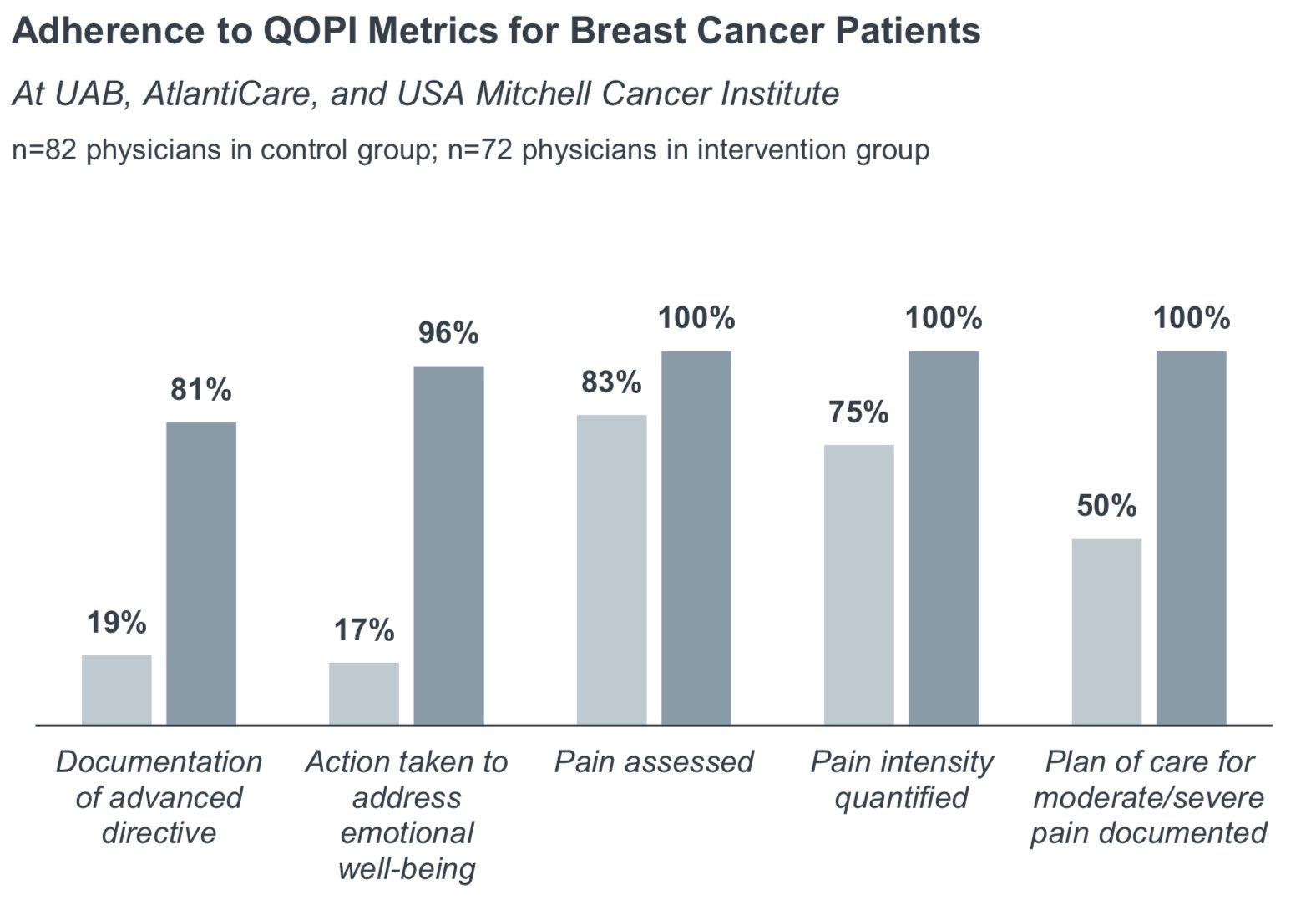
Since implementing Carevive, the three organizations have shown improvements in adherence to select Quality Oncology Practice Initiative (QOPI) measures.
Impressively, documentation of advanced directives increased from 19% to 81%. The organizations also measured significant improvements in metrics associated with pain and emotional well-being.
While documenting an advanced directive does not necessarily mean that patients have a comprehensive plan for care at the end of life, implementing reminders for physicians and standardizing these conversations for all patients can be an effective and meaningful step in the process of improving end-of-life care.
