Authors: Ruth A. Phillips, RN, MS, OCN, BCMAS Blue Spark Technologies, Cleveland, OH, and April Boyd, BSN, RN, OCN, Carevive, Boston, MA
Background
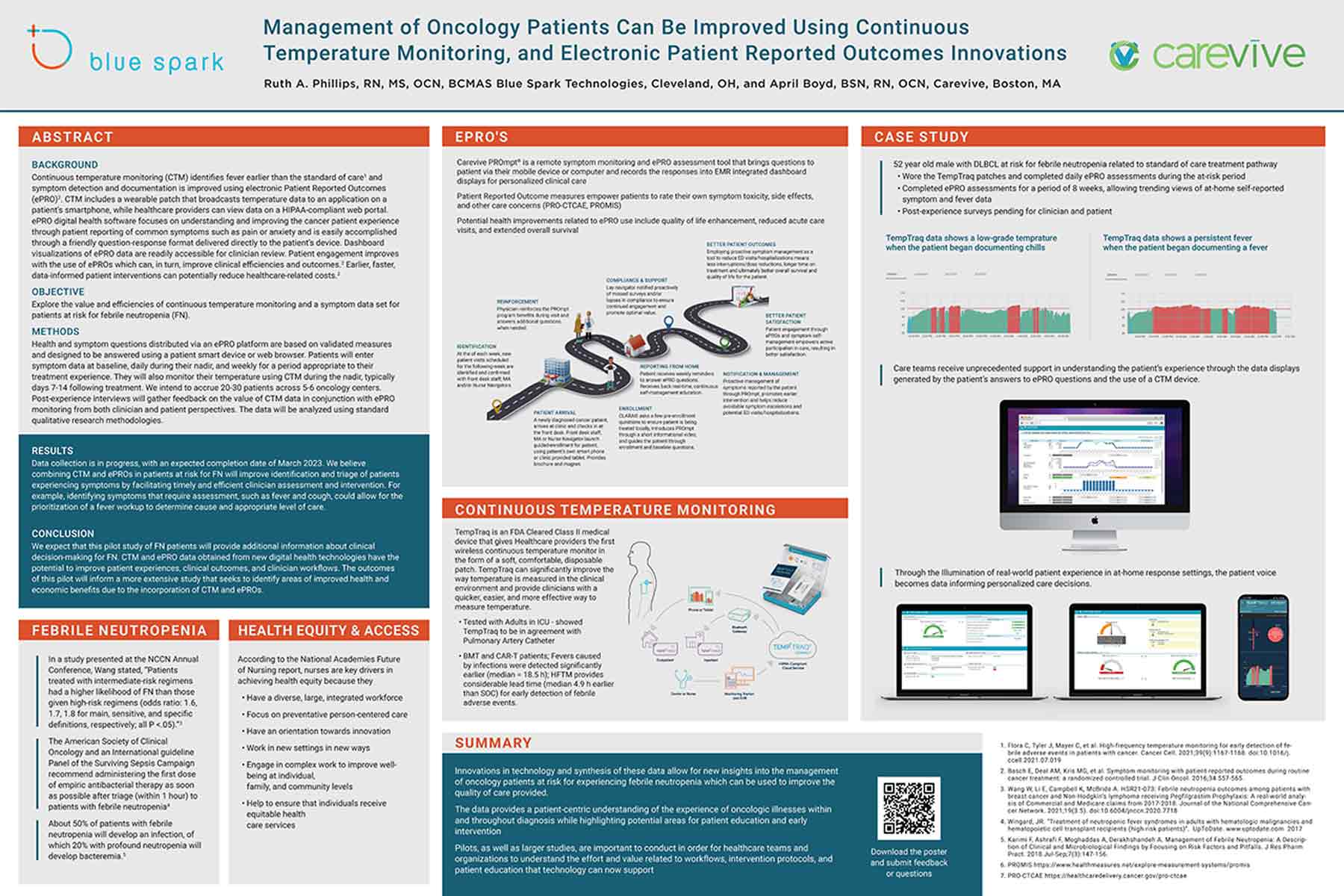
Continuous temperature monitoring (CTM) identifies fever earlier than the standard of care1 and symptom detection and documentation is improved using electronic Patient Reported Outcomes (ePRO)2. CTM includes a wearable patch that broadcasts temperature data to an application on a patient’s smartphone, while healthcare providers can view data on a HIPAA-compliant web portal. ePRO digital health software focuses on understanding and improving the cancer patient experience through patient reporting of common symptoms such as pain or anxiety and is easily accomplished through a friendly question-response format delivered directly to the patient’s device. Dashboard visualizations of ePRO data are readily accessible for clinician review. Patient engagement improves with the use of ePROs which can, in turn, improve clinical efficiencies and outcomes.2 Earlier, faster, data-informed patient interventions can potentially reduce healthcare-related costs.2
Objective
Explore the value and efficiencies of continuous temperature monitoring and a symptom data set for patients at risk for febrile neutropenia (FN).
Methods
Health and symptom questions distributed via an ePRO platform are based on validated measures and designed to be answered using a patient smart device or web browser. Patients will enter symptom data at baseline, daily during their nadir, and weekly for a period appropriate to their treatment experience. They will also monitor their temperature using CTM during the nadir, typically days 7-14 following treatment. We intend to accrue 20-30 patients across 5-6 oncology centers. Post-experience interviews will gather feedback on the value of CTM data in conjunction with ePRO monitoring from both clinician and patient perspectives. The data will be analyzed using standard qualitative research methodologies.
Overall results demonstrate the feasibility of gathering patient perspectives such as QoL preference, perceptions of curability, and treatment concerns in routine practice. While overall baseline differences did not vary significantly between groups, there was more concern about understanding treatment options and making the right decision in patients with hematologic versus solid tumors. Future research will explore changes in patient preferences and concerns over time as treatment progresses.
Results
Data collection is in progress, with an expected completion date of March 2023. We believe combining CTM and ePROs in patients at risk for FN will improve identification and triage of patients experiencing symptoms by facilitating timely and efficient clinician assessment and intervention. For example, identifying symptoms that require assessment, such as fever and cough, could allow for the prioritization of a fever workup to determine cause and appropriate level of care.
Conclusion
We expect that this pilot study of FN patients will provide additional information about clinical decision-making for FN. CTM and ePRO data obtained from new digital health technologies have the potential to improve patient experiences, clinical outcomes, and clinician workflows. The outcomes of this pilot will inform a more extensive study that seeks to identify areas of improved health and economic benefits due to the incorporation of CTM and ePROs.
References
1. Flora C, Tyler J, Mayer C, et al. High-frequency temperature monitoring for early detection of febrile adverse events in patients with cancer. Cancer Cell. 2021;39(9):1167-1168. doi:10.1016/j. ccell.2021.07.019
2. Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. 2016;34:557-565.
3. Wang W, Li E, Campbell K, McBride A. HSR21-073: Febrile neutropenia outcomes among patients with breast cancer and Non-Hodgkin’s lymphoma receiving Pegfilgrastim Prophylaxis: A real-world analysis of Commercial and Medicare claims from 2017-2018. Journal of the National Comprehensive Cancer Network. 2021;19(3.5). doi:10.6004/jnccn.2020.7718
4. Wingard, JR. “Treatment of neutropenic fever syndromes in adults with hematologic malignancies and hematopoietic cell transplant recipients (high-risk patients)”. UpToDate. www.uptodate.com 2017
5. Karimi F, Ashrafi F, Moghaddas A, Derakhshandeh A. Management of Febrile Neutropenia: A Description of Clinical and Microbiological Findings by Focusing on Risk Factors and Pitfalls. J Res Pharm Pract. 2018 Jul-Sep;7(3):147-156.
6. PROMIS https://www.healthmeasures.net/explore-measurement-systems/promis
7. PRO-CTCAE https://healthcaredelivery.cancer.gov/pro-ctcae

