Authors: Emelly Rusli MPH, Aaron Galaznik MD MBA, Debra Wujcik PhD RN Carevive by HealthCatalystTM, Boston, MA
Background
- Cancer care has moved beyond treatment response and survival to include the patient experience, that is, how the patient feels and functions during treatment.
- As such, treatment tolerability is no longer assessed only by the clinician but also to incorporate patients’ voices1-3.
- Patients with multiple myeloma (MM) are often on a lengthy course of therapy, emphasizing the importance of maintaining quality-of-life (QoL).
- Patient-reported outcomes (PROs) collected through remote symptom monitoring may facilitate early intervention when certain symptoms arise4 and bolster understanding of tolerability from the patients’ perspectives.
- Prior analysis showed some difference in QoL and physical function when MM patients experiencing a high degree of treatment bother.
- A recent publication by Brose et al. (2024) quantified patient-reported tolerability (PRT) in thyroid cancer.
- This study aimed to adopt this novel methodology to explore PRT in patients with MM using PROs collected in real-world clinical practice.
Methods
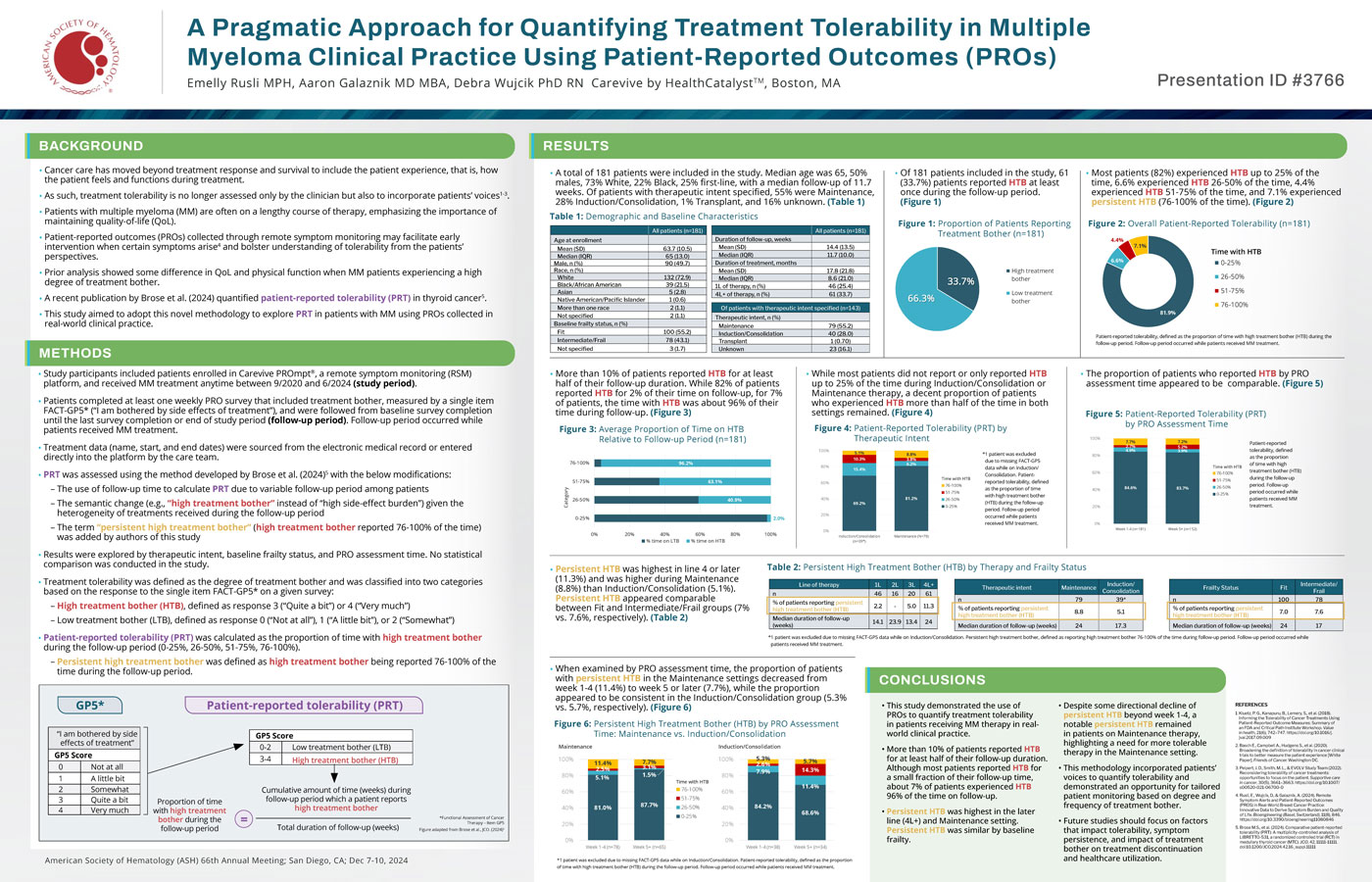
- Study participants included patients enrolled in Carevive PROmpt®, a remote symptom monitoring (RSM) platform, and received MM treatment anytime between 9/2020 and 6/2024 (study period).
- Patients completed at least one weekly PRO survey that included treatment bother, measured by a single item FACT-GP5* (“I am bothered by side effects of treatment”), and were followed from baseline survey completion until the last survey completion or end of study period (follow-up period). Follow-up period occurred while patients received MM treatment.
- Treatment data (name, start, and end dates) were sourced from the electronic medical record or entered directly into the platform by the care team.
- PRT was assessed using the method developed by Brose et al. (2024)5 with the below modifications:
- The use of follow-up time to calculate PRT due to variable follow-up period among patients
- The semantic change (e.g., “high treatment bother” instead of “high side-effect burden”) given the heterogeneity of treatments received during the follow-up period
- The term “persistent high treatment bother” (high treatment bother reported 76-100% of the time) was added by authors of this study
- Results were explored by therapeutic intent, baseline frailty status, and PRO assessment time. No statistical comparison was conducted in the study.
- Treatment tolerability was defined as the degree of treatment bother and was classified into two categories based on the response to the single item FACT-GP5* on a given survey:
- High treatment bother (HTB), defined as response 3 (“Quite a bit”) or 4 (“Very much”)
- Low treatment bother (LTB), defined as response 0 (“Not at all”), 1 (“A little bit”), or 2 (“Somewhat”)
- Patient-reported tolerability (PRT) was calculated as the proportion of time with high treatment bother during the follow-up period (0-25%, 26-50%, 51-75%, 76-100%).
- Persistent high treatment bother was defined as high treatment bother being reported 76-100% of the time during the follow-up period.
Conclusions
- This study demonstrated the use of PROs to quantify treatment tolerability in patients receiving MM therapy in realworld clinical practice.
- More than 10% of patients reported HTB for at least half of their follow-up duration. Although most patients reported HTB for a small fraction of their follow-up time, about 7% of patients experienced HTB 96% of the time on follow-up.
- Persistent HTB was highest in the later line (4L+) and Maintenance setting.
Persistent HTB was similar by baseline frailty. - Despite some directional decline of persistent HTB beyond week 1-4, a notable persistent HTB remained in patients on Maintenance therapy, highlighting a need for more tolerable therapy in the Maintenance setting.
- This methodology incorporated patients’ voices to quantify tolerability and demonstrated an opportunity for tailored patient monitoring based on degree and frequency of treatment bother.
- Future studies should focus on factors that impact tolerability, symptom persistence, and impact of treatment bother on treatment discontinuation and healthcare utilization.

